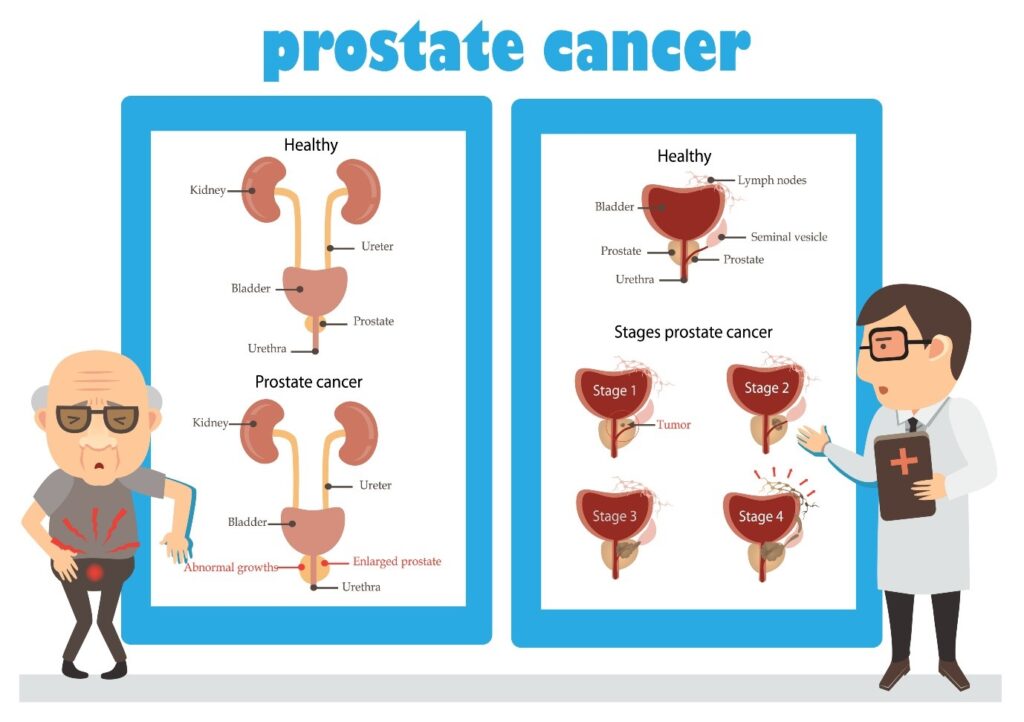
The prostate gland lies just below your bladder. Prostate cancer is caused when some cells in the prostate start to grow out of control. 1 in 9 men will be diagnosed with prostate cancer at some point in his life. Prostate cancer is rare in men under 50. The most common age of diagnosis is between 65 and 69 and the risk increases with age.
What are the risk factors for prostate cancer?
You are at higher risk of prostate cancer if you:
- Are aged 50 or older
- Have a close relative, for example, brother or father, who has had prostate cancer
- Are of black ethnic origin (double the risk)
- Diet is possibly a risk factor. As with other cancers, a diet high in fats and low in fruit and vegetables may increase the risk.
What are the warning signs of prostate cancer?
Unfortunately, there usually aren’t any early warning signs for prostate cancer. The growing tumour does not push against anything to cause pain, so for many years the disease may be silent. That’s why screening for prostate cancer is such an important topic for all men and their families.
In rare cases, prostate cancer can cause symptoms. Contact your doctor for an evaluation if you experience any of the following:
- A need to urinate frequently, especially at night, some- times urgently
- Difficulty starting or holding back urination
- Weak, or interrupted flow of urine
- Painful or burning urination
- Pressure or pain in the rectum
- Pain or stiffness in the lower back, hips, pelvis, or thighs
Remember: urinary symptoms don’t necessarily mean you have cancer. Prostatitis or BPH (Benign Prostatic Hypertrophy, also known as enlargement of the prostate) are benign diseases but can cause similar symptoms and are very common.
How is prostate cancer diagnosed?
If a doctor suspects that you may have prostate cancer, he or she will usually:
- Carry out a physical examination
- Do a blood test to measure the level of prostate specific antigen
- Carry out an MRI scan to produce a detailed image of the prostate and could prevent unnecessary biopsies for those with low-risk cancer.
- Carry out a biopsy if necessary
Treatment
Treatment options which may be considered include: surgery, radiotherapy, hormone treatment and, less commonly, chemotherapy. Often a combination of two or more of these treatments is used.
Treatment may aim to cure the cancer. In particular, the earlier the stage of the cancer, the better the chance of a cure.
Treatment may aim to control the cancer. If a cure is not realistic, with treatment it is often possible to limit the growth or spread of the cancer so that it progresses less rapidly.
What is the Outlook?
The outlook for prostate cancer is very variable. Some prostate cancers are slow-growing and do not affect life expectancy. On the other hand, some have already spread to other parts of the body when they are diagnosed. The response to treatment is also variable.
The specialist who knows your case can give more accurate information about your particular outlook and how well your type and stage of cancer are likely to respond to treatment.

Screening for prostate cancer
Discuss Screening With Your Doctor Starting at Age:
40 If you have a family history of prostate cancer or are African American
45 If you have no family history and are not African American
It should be noted that these recommendations apply to screening only—that is, testing of healthy men without symptoms. If you have any symptoms, you and your doctor will determine what the next steps should be.
Screening and Biopsy
What is a PSA Test?
The PSA test is the leading method of screening for prostate cancer. PSA, or prostate-specific antigen, is a protein produced by the prostate. During a PSA test, a small amount of blood is drawn from the arm, and the level of PSA, a protein produced by the prostate, is measured
When there’s a problem with the prostate—such as the development and growth of prostate cancer—more PSA is released. PSA screening can help catch the disease at an early stage when treatment may be more effective and potentially have fewer side effects. The PSA test may be done along with physical examination.
What if My PSA is High?
PSA screening is just the first step, alerting you and your doctor that more testing may be needed. If PSA is only slightly elevated, your doctor may recommend repeating the test a couple of weeks later. From there, other types of tests can help with the decision on whether you need a biopsy, including:
PSA velocity, or the rate of rise over time (faster increase means more risk)
PSA density, or the PSA per volume of prostate (higher density means more risk)
Magnetic resonance imaging (MRI) of the prostate
PSA blood test is also used to monitor treatment. If treatment is working and cancer cells are killed, then the level of PSA falls.
However, it is important to remember that some people believe that screening for all men may do more harm than good as a PSA test can have disadvantages and advantages as described in the table below. Therefore, it is important to discuss your medical history with your doctor before deciding to go for the PSA test
| ADVANTAGES | DISADVANTAGES |
| A PSA test can help pick up prostate cancer before you have any symptoms.
A PSA test can help pick up a fast-growing cancer at an early stage, when treatment could stop it spreading and causing problems or shortening your life. |
You might have a raised PSA level, even if you do not have cancer.
Many men with a raised PSA level do not have prostate cancer.
The PSA test can miss prostate cancer.
1 in 7 men with a normal PSA level may have prostate cancer, and 1 in 50 men with a normal PSA level may have a fast-growing cancer.
If your PSA level is raised, you may need a biopsy. This can cause side effects, such as pain, infection and bleeding. Not all men will need to have a biopsy. You might be diagnosed with a slow-growing cancer that would never have caused any problems or shortened your life.
Being diagnosed with cancer could make you worry, and you might decide to have treatment you do not need.
Treatments can cause side effects which can affect your daily life, such as urinary, and bowel problems.
|
Authored by:
Dr Zaineb Mohsin
MBBch, MSc in Critical care (UK), MRCP(UK)
Qualified as a physician, trained in Endocrinology and Diabetes from Imperial NHS Trust and currently working as a research fellow in Metabolic bone disease at Oxford University