WHAT IS ANEMIA?
Anemia is a medical term for low red blood cell count or haemoglobin.
WHY ARE RED BLOOD CELLS SO IMPORTANT?
Red blood cells contain a protein called haemoglobin, which has the important function of delivering oxygen from the lungs to the rest of the body. For men the normal haemoglobin reference range is between 130–180 g/L and for females the normal reference range is 120–160 g/L. New red blood cells are constantly required to replace old red blood cells with millions of red blood cells being released into the blood stream each day in healthy people. To produce new red blood cells the body needs key ingredients such as iron.
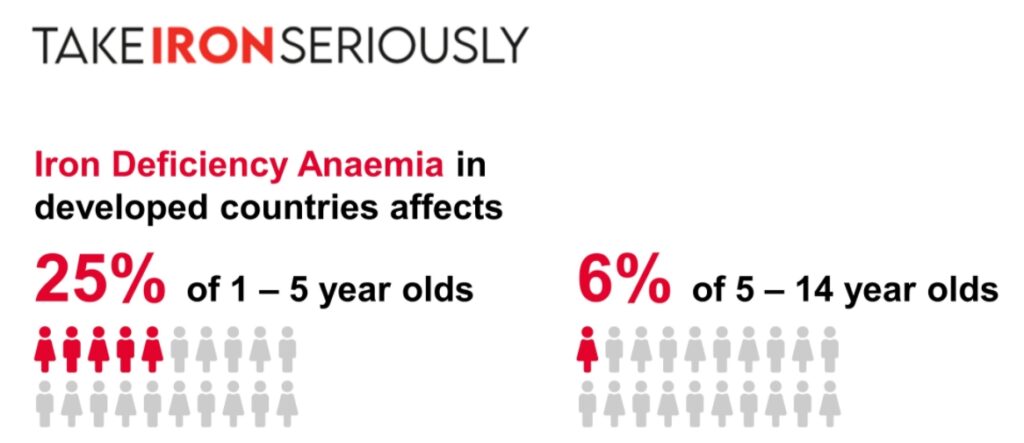
HOW COMMON IS ANEMIA?
Anemia affects more than two billion people globally, which is more than 30% of the total population. It is especially common in countries with few resources, but it also affects many people in the industrialized world.
ARE THERE DIFFERENT TYPES OF ANEMIA?
The most common cause of anemia is low levels of iron in the body. This type of anemia is called iron-deficiency anemia. Your body needs a certain amount of iron to make haemoglobin, the substance that moves oxygen throughout your body. However, iron-deficiency anemia is just one type. Other types are caused by:
- Diets lacking in or you cannot absorb vitamin B12.
- Diets lacking in or you cannot absorb folic acid, also called folate.
- Inherited blood disorders (like sickle cell anemia or thalassemia).
- Conditions that cause red blood cells to break down too fast (like haemolytic anemia).
- Chronic conditions causing your body to not have enough hormones to create red blood cells. These include hyperthyroidism, hypothyroidism and advanced kidney disease
- Blood loss related to other conditions such as stomach ulcers or bowel cancer.
AM I AT RISK OF ANEMIA?
Anyone can develop anemia, although the following groups have a higher risk:
Infants: Infants may get less iron when they are weaned from breast milk or formula to solid food. Iron from solid food is not as easily taken up by the body.
Children, ages 1 to 2 and adolescents: The body needs more iron during growth spurts.
Women: Blood loss during monthly periods and childbirth can lead to anemia. This is especially true if women have heavy periods.
People over 65: People over 65 are more likely to have iron-poor diets and certain chronic diseases.
Patients on blood thinners such as aspirin and warfarin or patients at risk of losing blood such as with bowel cancer or after major surgery
Medical conditions such as rheumatoid arthritis, liver or kidney disease, thyroid problems or inflammatory bowel disease (Crohn’s or ulcerative colitis)
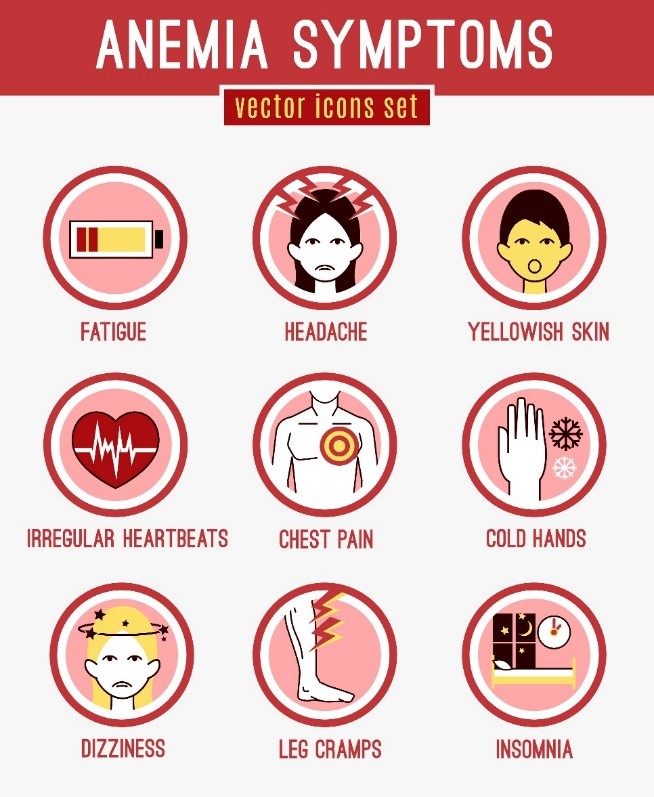
WHAT ARE THE SIGNS AND SYMPTOMS OF ANEMIA?
The signs and symptoms of anemia can easily be overlooked. In fact, many people do not even realize that they have anemia until it is identified in a blood test.
Several signs and symptoms occur in all types of anemia, such as fatigue, shortness of breath and feeling cold. Others include:
- Dizziness and light-headedness
- Pale skin colour
- A sore tongue
- Fast heartbeat
- Unusual cravings for non-food substances, such as dirt, ice, paint, or clay
HOW IS ANEMIA DIAGNOSED?
A blood Count is performed to determine if a person is anemic. This measure both the number and size of red blood cells and the amount of haemoglobin in a person’s blood.
Other tests to determine the cause would include:
- Vitamin B12 and folate levels
- Ferritin – checks the amount of iron
- Blood chemistry tests to demonstrate whether organs such as the liver and kidneys are working well.
- Blood tests looking for coeliac disease
Bone marrow biopsy
- This is rarely required and will only be carried out by a specialist in a hospital if a problem with the bone marrow is suspected.
Tests to see if there is bleeding somewhere – for example: Bowel investigations such as endoscopy and colonoscopy (camera tests looking at the stomach and large bowel)
HOW IS ANEMIA TREATED?
Finding out that you have anemia is just the beginning. Finding the cause of the anemia will lead you to the best treatment.
In many cases treatment prescribed by a doctor may be as simple as iron tablets if the cause is solely iron deficiency. Iron supplements can sometimes cause constipation, nausea, vomiting and diarrhoea, especially if supplements are taken on an empty stomach. Therefore, taking them with food, or switching to a liquid supplement can help. Taking vitamin C with iron can help its absorption.
Some cases of anemia may need a course of specific vitamins or more complex treatment such as a red blood cell transfusion, IV Iron or EPO (erythropoietin). Any underlying disease may also need to be treated. If you have been diagnosed with anemia or iron deficient anemia it is important that you are monitored by your GP. This can be done by having regular blood tests.
A note on Self-diagnosis
Taking iron supplements when you feel tired may not help unless you actually have iron deficiency. Unnecessary iron supplementation can interfere with your body’s absorption of other minerals. There may be another cause for your symptoms, which could be serious. Seeking treatment in the early stages of a disease can increase the chance of recovery and you may waste valuable time if you self-medicate rather than seeing your doctor.
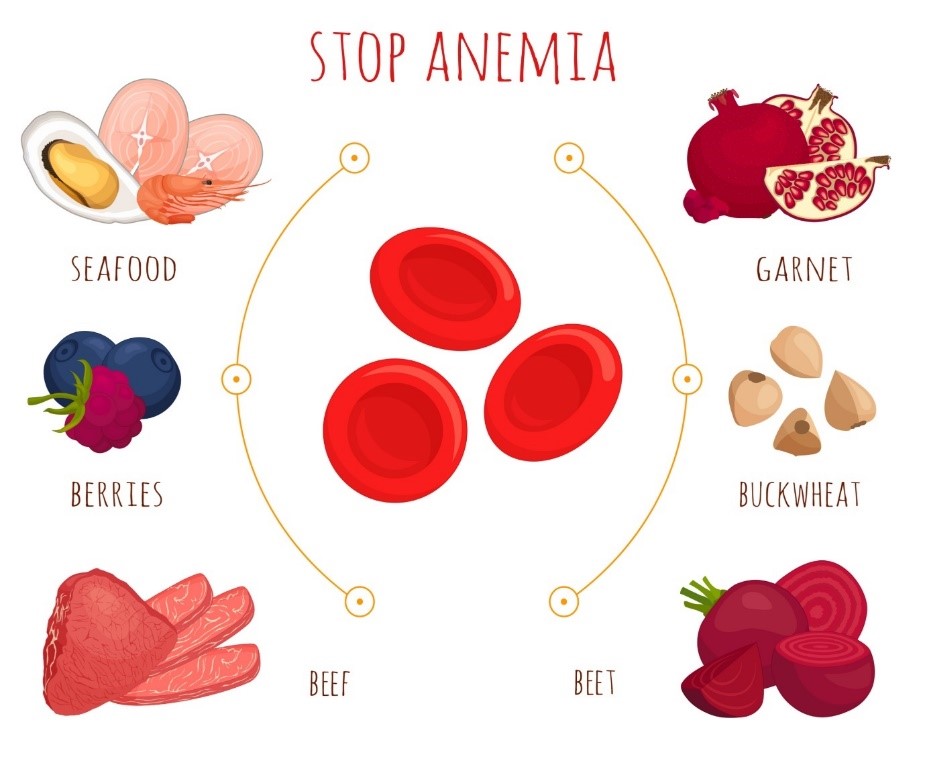
HOW CAN I PREVENT ANEMIA?
While many types of anemia (such as inherited causes) cannot be prevented, eating healthy foods can help you avoid both iron-and vitamin-deficiency anemia. Foods to include in your diet include those with high levels of iron (beef, dark green leafy vegetables, dried fruits, and nuts), vitamin B-12 (meat and dairy), and folic acid (citrus juices, dark green leafy vegetables, legumes, and fortified cereals). A daily multivitamin will also help prevent nutritional anemias; however, older adults should not take iron supplements for iron-deficiency anemia unless instructed by their physicians.
It is a good idea to get advice from your healthcare provider or perhaps from a registered dietitian about the best ways to eat when you have anemia.
It is important that you and your healthcare provider make decisions together about what works best for you. Make sure you ask all the questions that you have so you can be confident in moving forward.
WHEN SHOULD I SEE MY DOCTOR?
Talk to your doctor, nurse or midwife if you think you have any of the symptoms of anemia if you have noticed blood in your bowel motions or urine, or if you have persistent heavy periods.
Always discuss any alternative medicine, herbal preparation or over the counter treatments for anemia with a healthcare professional before taking them, as they may react with any prescribed medications.
Authored by:
Dr Zaineb Mohsin
MBBch, MSc in Critical care (UK), MRCP(UK)
Qualified as a physician, trained in Endocrinology and Diabetes from Imperial NHS Trust and currently working as a research fellow in Metabolic bone disease at Oxford University