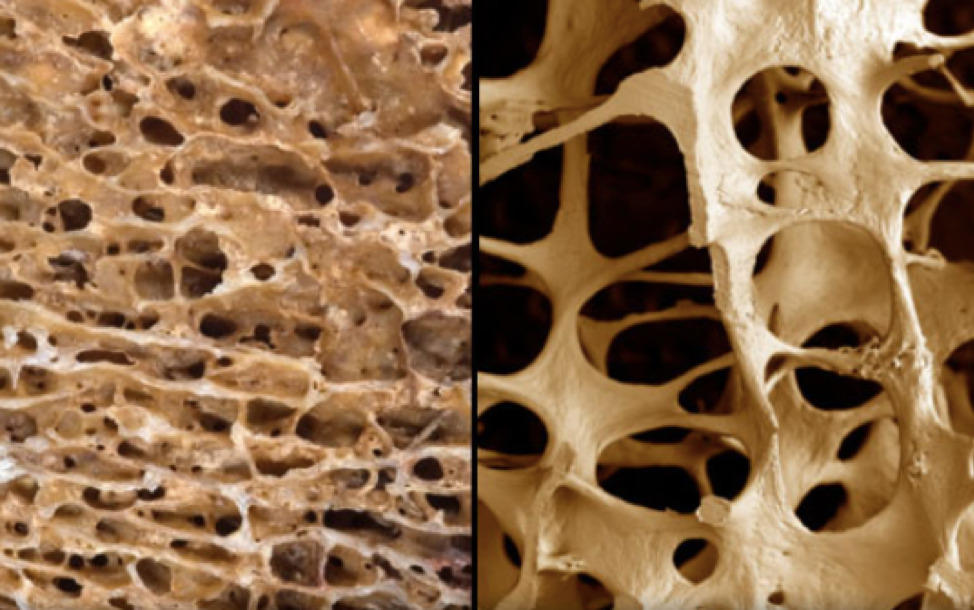
What is Osteoporosis?
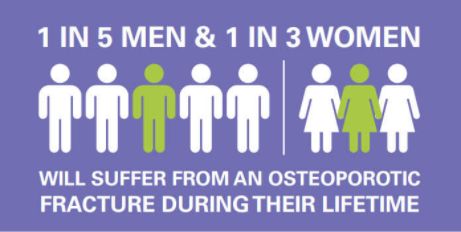
Osteoporosis is a silent disease of aging when the bones gradually become weaker and more porous. This makes them more likely to break. It is estimated that over the age of 50, one in three women and one in five men will suffer from an osteoporotic fracture over the remainder of their lifetime. It is often considered a silent disease as it is often diagnosed only after someone has had a fracture.
Why is it important to be aware of this condition?
- Osteoporosis is a common problem affecting 1 in 2 women over the age of 50 and 1 in 5 men.
- Osteoporosis is an expensive problem as the cost of hospital treatment and rehabilitation after a fracture can be considerable.
- Osteoporosis can lead to a loss of independence due to immobility. 33% of hip fracture patients are totally dependent or in a nursing home in the year after a hip fracture. A spine fracture can lead to back pain, stooping of the spine and loss of height which can be very distressing.
- Osteoporosis can lead to prolonged hospital stay. In women over the age of 45, fractures due to osteoporosis led to more days spent in hospital than for diabetes, heart disease and breast cancer combined.
- Osteoporosis can lead to death. About 20% of patients die in the first year following a hip fracture.
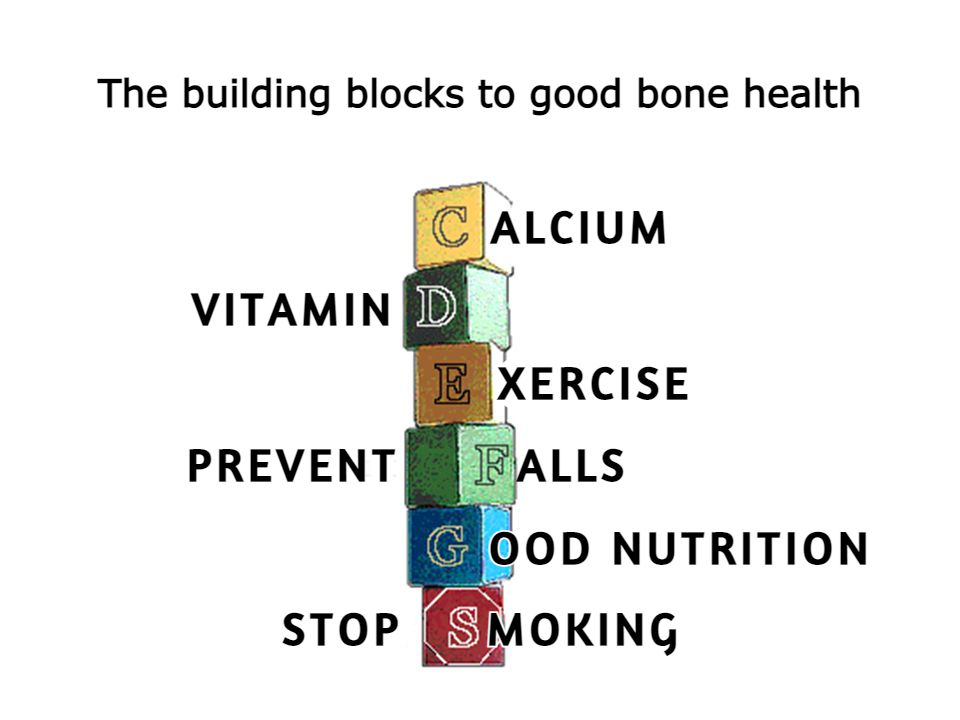
Prevention: What can I do to keep my bones strong at any age?
- Get adequate Calcium Intake: Ensure that you get enough calcium in your diet. The calcium requirements change with age, and there are useful calculators available that can guide you to the amount of calcium in your diet. Adult requirements for calcium range from 1000-1200 mg. If there is not enough calcium in your diet, you can take a supplement to ensure you are meeting your body’s requirements for this important nutrient.
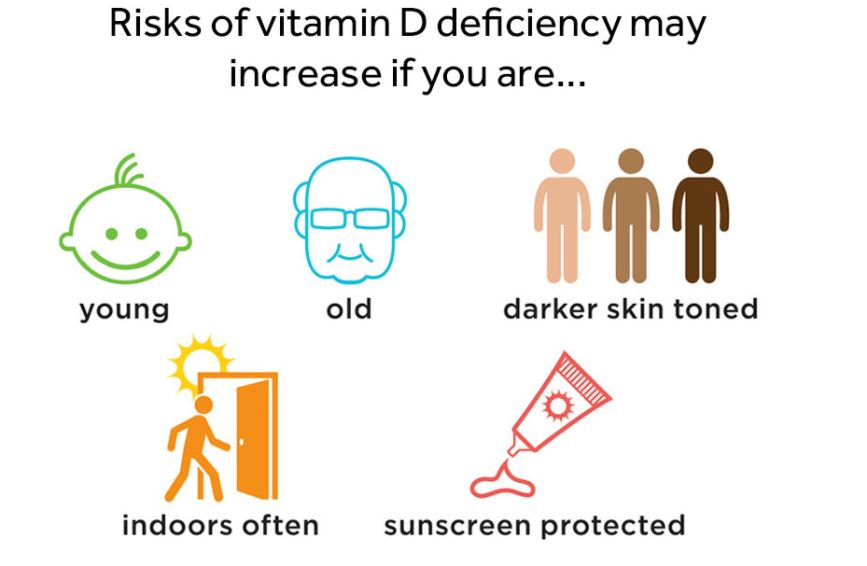
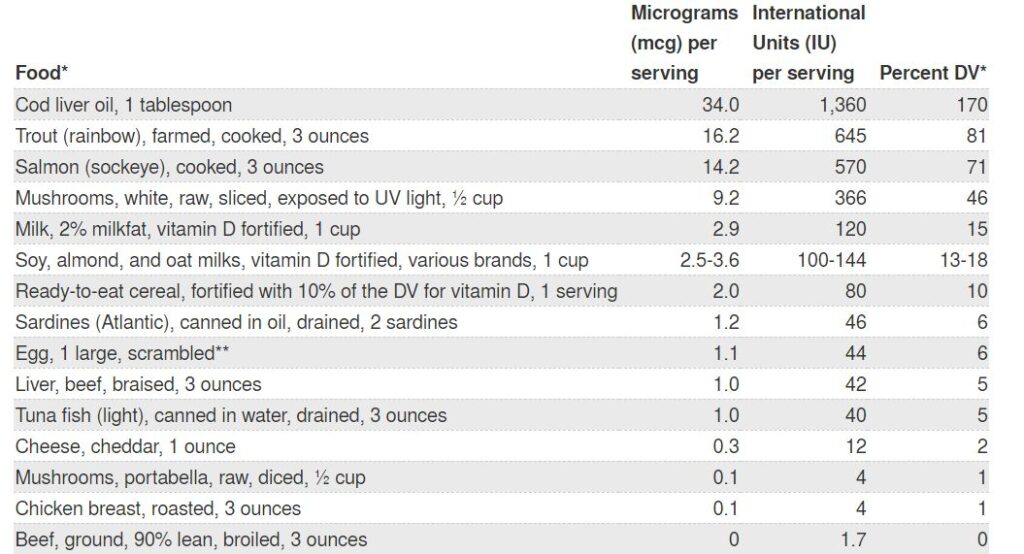
- Get enough Vitamin D: Vitamin D is essential for bones to be built properly and for them to remain strong. It is important to get enough sunlight on exposed skin and if you live in northern latitudes to take a vitamin D supplement. A supplement containing 800 – 1600 IU of vitamin D is usually recommended by your doctor or pharmacist. Vitamin D is present in small amounts in certain foods.
- Maintain a healthy body weight: A low body weight with a body mass index or BMI of less than 19, is associated with weaker bones.
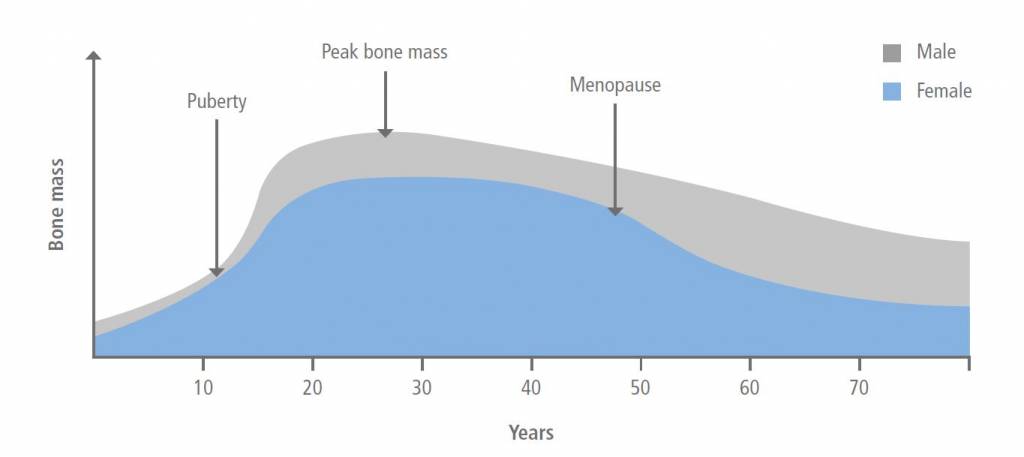
- Undertake regular exercise: Children and teenagers/young adults should exercise regularly as peak bone mass is attained in the early years up to young adulthood. Regular physical activity, especially weightbearing exercise, at any age is helpful in maintaining bone mass
- Falls prevention: If you feel that you are at risk of having frequent falls, you should seek help for walking supports or appliances around the home that will prevent you from falling and sustaining a fracture. You should check your vision and hearing regularly as problems with either can make you more likely to fall. Sometimes falls are caused by dizziness or abnormal sensation in the feet and treating this can help reduce your risk of falling.

Risks of Vitamin D deficiency may increase if you are:
- Young
- Old
- Darker skin toned
- Indoors often
- Sunscreen protected
Bone mass usually follows a cycle where bone is built during the first two decades of life until peak bone mass is reached in the mid-twenties. Following this bone mass remains stable and then gradually starts to decrease. After menopause women have a sharper decrease due to loss of oestrogen. Men attain a higher peak mass than women and so the risk of osteoporosis is lesser in men.
How do I know if I am at risk for osteoporosis?
Unfortunately, everyone’s bones get weaker as they get older, so age is a risk factor for osteoporosis. Women are also at higher risk as they attain a lower peak bone mass than men. Other considerations are:
- If you have underlying medical conditions that put you at a risk for a low bone density such as rheumatoid arthritis, type 1 diabetes, Crohn’s disease, Coeliac disease, chronic liver disease, chronic kidney disease or an over-active thyroid.
- If you have used steroids (such as prednisolone) for more than 3 months at a dose of
- If your parents have had a hip fracture.
- If you smoke or consume excess alcohol.
- If you use medications that block the action of oestrogen or testosterone such as those used in the treatment of breast and prostate cancer respectively.
- If you have suffered from a fracture, especially with minimal trauma (such as a bump or a fall), you are at a very high risk of developing further fractures.
If you have any of the above conditions, you should talk to your doctor about assessing your bones. If you prefer an informal risk assessment, the International Osteoporosis Foundation has a risk calculator you can use to determine your personal risk. You can find this here.
How can osteoporosis be diagnosed?
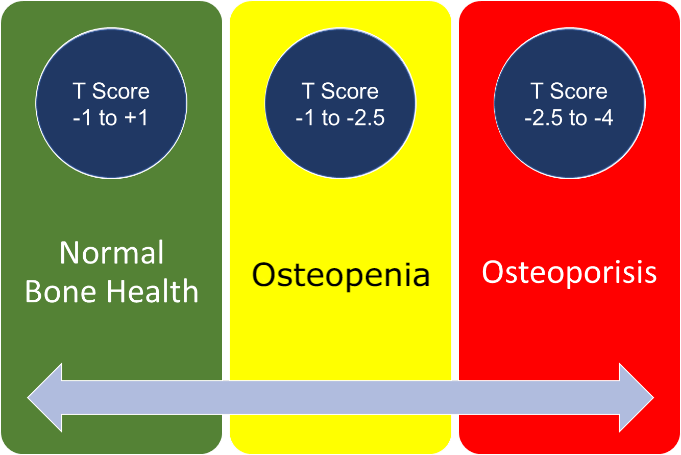
Osteoporosis can be diagnosed by a low dose x ray machine called a DEXA (dual-energy X-ray absorptiometry) scanner. In some countries (e.g. U.S.A.), BMD testing is recommended for all women and men at age 65, regardless of whether they have risk factors. It is a painless procedure where an open X-ray machine is used to calculate the density of the bones at the hip and spine.

A number worse than -2.5 at any site confirms the diagnosis of osteoporosis. A number between -1.5 and -2.5 indicate the bones are weaker than the general population. We call this osteopaenia.
In some cases, the doctor may also carry out an assessment called FRAX. This looks to see if you have a high risk of getting a fracture in the future and takes into consideration your age, gender, medical history, medication history and your DEXA report. This helps guide the doctor to the best treatment option for you.
If you are over the age of 75 and have fractured the bones in your back, hip, wrist, shoulder bone or ribs with minimal trauma such as a fall at home, you do not need a DEXA scan to diagnose whether you have osteoporosis, as the fracture itself confirms the presence of the disease.
How is osteoporosis treated?
Osteoporosis is usually treated by means of two classes of medications. The first class prevents bone from being broken down. They are called “anti-resorptive” drugs (anti-against, resorptive-being broken down). They include bisphosphates and a newer drug called denosumab. Raloxifene and Strontium are other agents that are sometimes used.
Bisphosphonates (which include drugs such as alendronate, risedronate, zoledronate) are the most common medications prescribed for osteoporosis. They reduce the risk of fractures by about 50% The bisphosphonates have uncommon side-effects, in that out of every 1000 teeth extracted one may have delayed healing (a condition called osteonecrosis), and out of every 100 fractures it prevents, it may cause an atypical fracture. Bisphosphonates should not be given to patients with severe renal failure (an eGFR less than 35).
The second class of medications are anabolic drugs (medications that build new bone). These medicines are usually reserved for patients with severe osteoporosis (a value of -4.5 or more on the bone density scan or if patients cannot tolerate other medications). This includes drugs such as teriparatide and romosozumab.
For women, Hormone Replacement Therapy is sometimes used when menopause is reached to help with symptoms of the latter. This can lead to improvement in BMD. However, it is only used for about 10 years, so is not a long-term solution in the management of osteoporosis.
I am worried I may have osteoporosis. What should I do next?
- Speak to your doctor who will likely request a DEXA scan or carry out a FRAX assessment. He will also carry out blood tests to check your calcium, vitamin D, kidney function and other tests based on your medical history.
- Based on the DEXA scan and FRAX assessment, treatment recommendations will be made.
- If treatment such as bisphosphonates are recommended, it is important that you stick with the treatment as it will significantly reduce your risk of fractures.
- Ensure that you are taking enough calcium in your diet and continue Vitamin D supplementation to keep your levels in the normal range. Implement lifestyle measures as described above.
- Continue to keep yourself informed from reliable resources such as the International Osteoporosis Foundation (IOF), the Royal Osteoporosis Society (ROS) and the National Osteoporosis Foundation (NOF).
Where can I find more information about osteoporosis?
General information about osteoporosis can be found on the Royal Osteoporosis Society. The International Osteoporosis Foundation has very useful for information for patients and doctors with representation in several countries around the world. There are useful videos on every aspect of bone care from prevention to treatment of this condition. There are also helplines you can phone to speak to experienced volunteers if you or a loved one has been recently diagnosed with osteoporosis. This will incur a charge if you live outside the UK.
Authored by:
Dr Zaineb Mohsin
MBBch, MSc in Critical care (UK), MRCP(UK)
Qualified as a physician, trained in Endocrinology and Diabetes from Imperial NHS Trust and currently working as a research fellow in Metabolic bone disease at Oxford University.